Finally scientists and researchers are one step closer to a cure for HIV – a study has found. The latest research shows that molecules were tested on mice and diminished the HIV virus in the HIV infected mice by 80 to 95%. The new findings were published in the journal Molecular Therapy. It incorporates an engineered molecule called a CAR – chemeric antigen receptor – that is added to the blood-forming stem cells to repair and re-empower the immune system’s response to the virus.
“We hope this approach could one day allow HIV-positive individuals to reduce or even stop their current HIV drug regimen and clear the virus from the body altogether. We also think this approach could possibly be extended to other diseases,” said Scott Kitchen, the study’s lead author and a member of the Broad Stem Cell Research Centre and UCLA AIDS Institute. He is also an associate professor of medicine in the division of haematology and oncology at the David Geffen School of Medicine at UCLA.
The mice used in the research was genetically engineered to mimic a human’s immune system and then infected with HIV. Kitchen and his colleagues then transplanted CAR-modified blood stem cells into the mice. The CAR molecule is inserted into blood-forming stem cells. These blood-forming stem cells can turn into any type of blood cell, and in the case of the HIV virus has to turn into T cells (the white blood cells central to the immune system) in order to strengthen the immune system (weakened by the virus) and fight the virus. The HIV virus is too strong and mutates too fast for T cells to fight the virus. In the lab test result proved that these new two-part receptors called CARS, successfully turned into functional T cells and decreased the HIV levels of the infected mice.
This brings hope for one of the world’s biggest problems – HIV/AIDS! If a mouse with a human’s immune system is able to fight the virus after the CAR molecule is inserted, then there is a big possibility that this could work in humans once inserted into the blood-forming stem cells of infected humans.
T cell receptors tested in previous tests conducted by the same researchers at UCLA could not prevent HIV from mutating away from the T cells. The other obstacle they faced during these tests, were that the T cell receptors they used had to be adjusted to each patient’s body. In the case of the CAR molecule, it has been found to be universally adaptable (for the moment to the mice only) but could be trialled on humans across the border within the next five or ten years if ongoing tests prove positive. The CAR tests have only been done on mice so far; it has not been approved by the Food and Drug Administration for the use in humans yet.
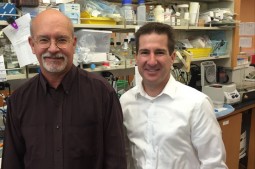 The scientists – led by Jerome Zack (left) and Scott Kitchen (right)
The scientists – led by Jerome Zack (left) and Scott Kitchen (right)
Professor Jerome Zack is a colleague of Kitchen and a co-author of the study. He is a professor of medicine and of microbiology, immunology and molecular genetics in the UCLA David Geffen School of Medicine and a co-director of the UCLA AIDS Institute. The Professor said: “Despite increased scientific understanding of HIV and better prevention and treatment with available drugs, a majority of the 35 million people living with HIV, and millions more at risk of infection, do not have adequate access to prevention and treatment, and there is still no practical cure. With the CAR approach, we aim to change that.” Professor Zack is also affiliated with UCLA’s Jonsson Comprehensive Cancer Centre and a member of the Broad Stem Cell Research Centre.
In 1999 international researchers discovered that the HIV-1 strain (the predominate strain in the developed world) originally came from a type of chimpanzee in West Africa and it is believed that hunters were infected when they went hunting these primates. The virus found in the chimpanzees (originally called simian immunodeficiency virus or SIV) eventually spread across Africa and other parts of the world. The first human infected with HIV-1 was a man, who came from Kinshasa, in the Democratic Republic of the Gongo. In 1959 a blood sample taken from him detected the virus and revealed upon genetic analysis that it came from a single virus dating back to the late 40/early 50’s. In the mid to late 70’s the virus was detected in the United States. In 1979-1981 rare types of illnesses were reported amongst homosexual men in Los Angeles and New York to doctors and it was found that HIV was the cause.
In 2014 it was estimated that 36.9 million people were living with HIV/AIDS (according to estimates by WHO and UNAIDS) and in the same year 1.2 million people died of AIDS-related causes. Then there are still the millions who are at risk of being infected and those who do not know that they are infected already. HIV/AIDS is an incurable disease (for the moment it still is) because once it enters the body it attacks the T cells that we need to fight illnesses with. The T cells have to attack viruses or infections that enters’ the body, but because the virus has the ability to mutate it kills faster than it gets killed and the T cells eventually become powerless. Eventually the body can’t fight the simplest of infections and the HIV infected person can die of any kind of illness like for example cancer, colds, flues and pneumonia. These opportunistic infections became known as AIDS (acquired immunodeficiency syndrome) in 1982 and a year later in 1983 HIV, the virus that causes AIDS, were discovered. HIV (human immunodeficiency virus) was previously known as HTLV-III/LAV (human T-cell lymphotropic virus-type iii/lymphadenopathy-associated virus).
For people who are living with HIV/AIDS, there is antiretroviral therapy (ART) to fight the virus from spreading and causing further damage to the body. Antiretroviral drugs (ARV’s) are given to people who are infected with HIV and combining more than one of these ARV’s would give you a better chance of surviving. Once you start taking the ARV’s you have to take it once a day for the rest of your life. Presently there are more than 20 approved antiretroviral drugs on the market and these can be used in combination therapy or highly active antiretroviral therapy (HAART) where two or more different types of antiretroviral drugs are taken in combination. There are six major drugs used to treat HIV/AIDS and these are called Entry Inhibitors, Fusion Inhibitors, Reverse Transcriptase Inhibitors, Integrase Inhibitors, Protease Inhibitors and Multiclass Combination Products.
The study’s first author was Anjie Zhen, a postdoctoral fellow at UCLA in the Division of Haematology/Oncology, the UCLA AIDS Institute and the Broad Stem Cell Research Center. The work was supported by the National Institute of Allergy and Infectious Disease, the National Institutes of Health, the UCLA Centre for AIDS Research, the California Institute for Regenerative Medicine, the University of California Multicampus Research Program and Initiatives, the California Centre for Antiviral Drug Discovery, the California HIV/AIDS Research Program and the UCLA Broad Stem Cell Research Centre.
Let’s hope that the CAR molecule proves successful in the next round when they start testing humans. Thumbs up for the lab mice!










This is good news